Could You Have A ‘Copper Hangover’ From Pregnancy?
There is a strong relationship between copper levels in the body and the hormone oestrogen. Pregnancy is a time when oestrogen levels rise significantly. When oestrogen levels rise, so do copper levels. Copper levels, particularly in excess play a role in postpartum mental health disorders.
COPPER & PREGNANCY
During pregnancy the oestrogen level steadily rises over time, reaching 30-fold levels by birth! Elevated oestrogen (to some degree) is not limited to pregnancy, it's also seen in puberty, with the contraceptive pill and some types of menopause hormone therapy/HRT.
And as oestrogen levels rise, copper levels rise and maternal zinc levels fall.
This copper rise (2-3x the preconception level) is essential for the body in pregnancy. As copper promotes the production of blood vessels which, during pregnancy is happening a lot! For the mother, for a healthy placenta and a healthy baby.
Copper is built up by the baby during pregnancy; stockpiled in the liver. This is a normal physiological process because copper is important for building new blood vessels.
Outside of pregnancy, elevated copper (and more-so copper toxicity) and its vascular promoting properties can drive women's health issues such as endometriosis, fibroids and reproductive organ tumours (e.g. cervical, ovarian, uterine, vaginal). It's also linked to mental health issues (more on this below) and inflammatory conditions.
POSTPARTUM
Ideally after pregnancy, the copper levels decrease dramatically. It's thought this massive drop occurs (or should occur) within the first 24 hours after the birth. If it stays dangerously high this can even lead to severe postpartum psychosis. This is because copper toxicity has dramatic effects on the brain's chemicals.
The body's ability to clear this (now) excess copper after pregnancy depends on a few factors. These include having adequate zinc levels, adequate Vitamin A levels and if the mother's 'copper detox mechanism’ is not impaired by any genetic 'snips'.
The accumulation of high levels of copper can also compound over pregnancies. As explained, with each pregnancy the copper level (at least) doubles then ideally should return to a healthy baseline. If it doesn't, a mother’s 'baseline' will remain higher than normal. Then 1-2 years later, perhaps another pregnancy occurs that will shoot up her copper levels again, but this time even higher because her baseline level was higher to start with. Her postpartum copper levels do decrease, but again not to optimal, healthy levels because her baseline copper level was higher than normal to begin with. This copper state worsens again with the next pregnancy. All in all, this puts a mother at a higher risk of postpartum mood disorders associated with high copper levels.
This is not a new finding. A study published in the Journal of Trace Elements in Medicine and Biology in 2007 found 'women with a history of postpartum depression tend to have unusually high levels of copper in their blood.'
MENTAL HEALTH
If the copper levels do not decrease on their own, the copper excess levels in the brain can impact the mood-regulating neurotransmitters; dopamine and norepinephrine (adrenaline).
Too much copper tends to force or push the conversion of dopamine into norepinephrine, which alters the delicate balance of these two mood-regulating neurotransmitters. And as dopamine levels decrease, the norepinephrine levels increase.
This can manifest as postpartum mood disorders including anxiety, panic, and depression. Also, when there are high levels of copper in the body, this acts as an antagonist to the zinc levels in the body. This will drive and/or maintain a zinc deficiency. Zinc is essential for a multitude of actions in the body, one of which is mental health.
Stress is a major factor that affects copper balance (hello postpartum). Under stress, the body loses large amounts of zinc and magnesium from tissue storage. This shortage of zinc allows copper levels to elevate.
Copper also binds to GABA receptors. This interferes with the action of this key calming neurotransmitter (GABA) and contributes to anxiety and depression. As well as anger and frustration.
As copper levels rise in the body, potassium levels drop and calcium levels increase. This can create an ‘adrenal burnout’ scenario.
Copper is also involved in how we absorb and utilise the iron in our body. We need copper for this, but when there is too much copper it will have deleterious effects on iron metabolism. Iron deficiency also affects mental health.
NATUROPATHIC CONSIDERATIONS
Copper overload and/or zinc deficiency is something I always consider with postpartum mood disorders. Even if 'postpartum' was years prior.
I will often look back to the preconception stage. If there were years of hormonal contraceptive use (e.g the Pill or copper IUD) before pregnancy, this can increase various mineral deficiencies and may have contributed to the copper load. Hence, the importance of preconception care.
The body has an in-built defence system to protect us from absorbing too much copper. It’s called the Metallothionein system. This system is a highly zinc-dependent system, therefore will only work well when there’s adequate zinc (and cysteine).
Therefore, having a zinc deficiency (also alongside a vitamin B6 and vitamin C deficiency) will contribute to copper accumulation.
Having hormonal imbalances that create an oestrogen-dominant state will further drive copper excess or toxicity. Therefore, this needs to be investigated and addressed as part of the holistic approach.
COPPER SOURCES
It’s important to look for external sources of copper. A common source is drinking water that runs through copper pipes. Copper water pipes leach minute amounts of copper into the water continuously. This piping is common in houses built before 1980. Even if this is a minor source, if there is already a copper overload, this can ‘tip over’ the copper level.
Swimming in pools or spas can also be a source of copper with frequent use. This is due to copper sulfate being added as an algicide.
Environmental xeno-oestrogens are also linked to copper excess. These are synthetic chemicals released into the environment as pollutants from agricultural spraying (pesticides and herbicides), from industrial processes, food storage procedures and waste disposal (PCBs and dioxins). These persistent organochlorine pollutants are also generally passed up the food chain. Often found in fatty meat and fish, and in dairy products (milk, butter, and cheese) in the fat content.
They’re also found in makeup, personal care products, and cleaning chemicals in the home.
TESTING
The ratio of copper and zinc can be assessed through a blood test, and ceruloplasmin (the 'copper-carrying protein') also needs to be tested.
From these, the percentage of free/unbound copper can be calculated. It’s the free copper that is causing the problem (more on this below). Someone can have a normal copper level result, yet still have very high free copper.
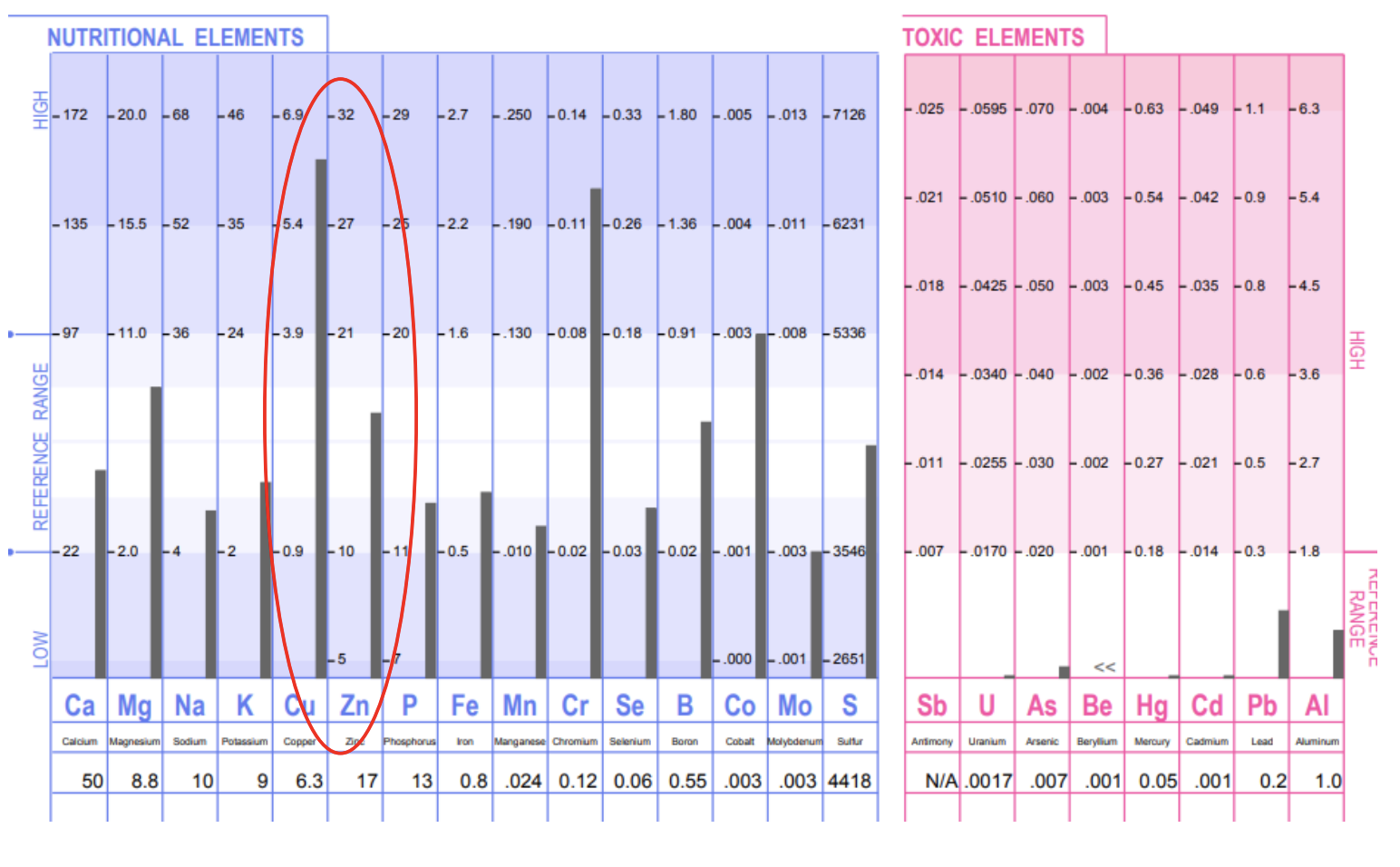
Also, Hair Tissue Mineral Analysis (HTMA) can be of great value assessing the amount of copper stores in the body, as hair is a storage tissue. It can also show the relationship of the copper level to other minerals such as zinc and iron.
I'll often see high copper alongside low zinc, low iron, low manganese, low molybdenum and low potassium.
There is some debate regarding the best way to test for copper toxicity; through blood or through a HTMA. Sometimes there will be a consistent result of high copper to low zinc across both a blood test and a HTMA. Yet, sometimes (a lot of the time) a blood test looks fine, yet there is a stockpile of copper in the tissues revealed through a HTMA. If excess copper or copper toxicity is suspected, the ideal scenario is to do both.
Hair Tissue Mineral Analysis Report showing high copper
WHAT IS CERULOPLASMIN?
Ceruloplasmin is a 'copper-carrying protein' in the body.
Roughly 95% of the copper found in the blood is bound to ceruloplasmin. This should also be tested when assessing copper levels to look for clues as to why there may be a copper issue.
Ceruloplasmin is made in the liver. It helps protect the body from too much 'free-floating, unbound copper'. It’s similar to a bus; picking up ‘copper passengers’ to avoid them spilling out over the streets and the neighbourhood causing havoc! In the body, this is known as oxidative stress and inflammation. High levels of unbound copper is also associated with various neurological disorders.
Ceruloplasmin carries these ‘copper passengers' around the body in a safer (bound) form. This way it can deliver (let off) the copper where it’s needed in the body. The body also likes to use copper from this ceruloplasmin form.
Ceruloplasmin is also integral to how the body utilises iron; helping in both the transport and regulation of iron levels in the body.
It’s important to note, adequate dietary protein is required to make ceruloplasmin.
When testing copper and zinc in the blood, it’s important to also test ceruloplasmin to see the relationship between the copper level and the ceruloplasmin. Having low ceruloplasmin can point to genetic conditions called Wilson or Menkes disease, a copper deficiency, or other medical conditions affecting the liver or kidneys. This will also allow unbound copper to circulate freely in the body - which is highly problematic.
THE ROLE OF VITAMIN A
Vitamin A in its natural, preformed form retinol, helps regulate copper in the body. It does this by helping the body convert copper into ceruloplasmin. Therefore, if there’s not sufficient Vitamin A in the diet this can contribute to, or worsen high (free) copper levels.
One study found that one-third of pregnant women were borderline deficient, despite having access to plenty of vitamin A-rich foods.
There once was a huge fear and controversy around ‘vitamin A in pregnancy’ and its toxicity causing birth defects. This toxicity was linked to high-dose, synthetic, supplemental form of vitamin A.
Yet, the naturally occurring vitamin A found in foods such as eggs, organ meats (liver/pâté) or liver supplements, cod liver oil and full-fat dairy, provide true preformed vitamin A in the form of retinol.
When there’s a suspected copper issue, it’s useful to zoom out and consider all the factors involved in copper levels in the body.
WHAT CAN BE DONE
If testing reveals an issue with copper, zinc and/or ceruloplasmin then it’s important to find the root cause of this imbalance.
Simply taking a zinc supplement to counteract the high copper is not the answer. It can mobilise copper very quickly. This ‘copper dumping’ can worsen symptoms and so, is not recommended.
It’s also important to check iron levels, as mineral imbalances in the body often have ripple effects. Plus, if there is low iron then taking a zinc supplement can worsen this. Other nutrients besides zinc (as mentioned above) are needed to normalise copper levels in the body.
With high copper there is often low levels of manganese and molybdenum. A HTMA will often reveal this pattern.
The best approach is to identify and rectify the source/s of copper that are contributing to the excess. As well as working on a slow and steady ‘copper detox’. It’s also favourable to help prepare the body for the upcoming mobilisation of excess copper.
Nutritional therapy is powerful here, plus antioxidant support (eg. vitamin C, vitamin E, NAC and glutathione). This is because copper is highly pro-oxidative and through its elimination it will tax the body’s antioxidants. It can also affect sensitive tissues such as the thyroid gland.
As copper is stored in the liver (and brain) and is eliminated via bile, both liver and gallbladder support is important. Herbal medicine and certain nutrients (eg. taurine) are very helpful here.
Of course, it’s essential to remove copper sources from the environment, especially daily drinking water sources. Avoid drinking public system tap water as much as possible. Use a quality water filtration system for drinking (eg. Zazen) and also use this water for cooking. Installing a shower filter that eliminates copper (and chlorine/chlorine gas, water-soluble lead, mercury, nickel and chromium) is also highly recommended.
What about food sources of copper? Avoiding copper-rich foods whilst actively trying to detox copper toxicity can add more stress than benefit. I take this on a case-by-case basis.
CONSIDERATIONS
There is a myriad of factors that contribute to a mother’s mental health in postpartum. Considering and evaluating the role of copper, zinc and ceruloplasmin may provide some significant clinical insights. This information enables a personalised treatment approach that ultimately aims to address the underlying imbalances (root cause) that are contributing to a mother’s symptoms.